The last couple of years has been eye-opening for the healthcare industry. It brought the importance of effective infection control in healthcare facilities to the forefront. While doctors and hospital administrators work tirelessly to treat patients, healthcare architects ensure that they provide the proper support by creating innovative designs for hospital environments that improve infection prevention and control at the health facilities.
We know that design impacts disease control. That is why we work in collaboration with the hospital infection control team to reduce infection transmission and make hospital environments safer for both patients and staff. Here are 5 tips to ensure that your healthcare facility is designed, keeping infection control practices in mind, so that providers and patients can stay safe and sterile!
1. Keep it Simple
Identify the essential and eliminate the rest. Studies show that a minimalist design, with fewer flat surfaces, helps to decrease the transmission of infectious agents like bacteria, viruses and fungi. Monolithic surfaces minimize or eliminate joints that can harbour infections.
In hospital wards, where there is a lot of movement and activity, proper design of the patient headwall and placement of medical equipment while providing adequate storage can go a long way in minimizing clutter, reducing the risk of infection transmission and improving operational efficiency.
2. Keep it Clean
It is essential to keep surfaces and floors as clean and sterile as possible. Here are two factors that could help.
a. Resilient surfaces
As a practice, hospital floors and surfaces are exposed to frequent cleaning with harsh chemicals. So, we need materials that are resilient enough to withstand these factors, and that won’t easily deteriorate or crack or break so that we can clean them appropriately. Hospitals are also high traffic areas with increased movement, especially during emergencies. We need surfaces that are strong and durable enough to face these harsh conditions.
b. Anti-microbial finishes and materials
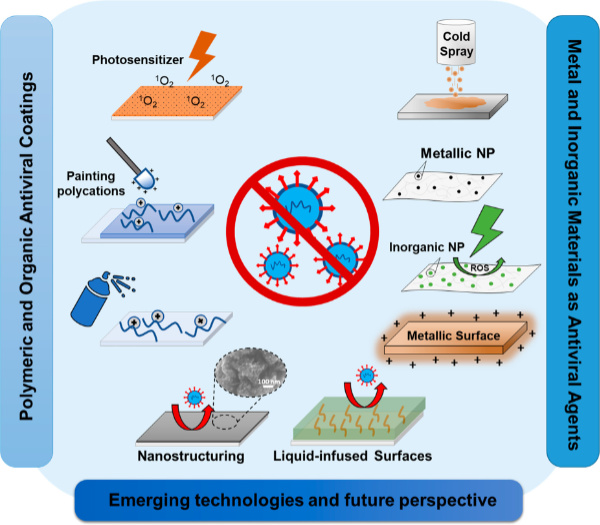
Considerable industry research has been done to find solutions that prevent bacterial transmission and biofilm formation by killing microbes or reducing their attachment to clean surfaces. These include surface-bound active antimicrobials, and biocidal coatings or passive pathogen-repellent surfaces developed using nanomaterials, chemical modifications, and micro- and nano-structuring.
3. Keep it Contained
Isolation areas are designed for the care of critically ill patients who need to be isolated from the rest of the patients and all other people visiting or working in the healthcare centre. The doctors, caregivers and anyone else coming in close contact with the patients are protected from infection or contamination.
The extent of isolation required can be broadly classified as per the three types of patients, viz. patients who only need additional monitoring, patients who are susceptible to infection and patients who have air-borne, contagious diseases. The primary focus must be on zoning, ventilation and sterilisation. How can we build robust isolation centres that serve the purpose?
a. By constructing air-locked lobbies and maintaining pressure differential in these areas. Airlocks prevent the passage of air between the contained area and its adjoining areas.
b. By ensuring an adequate number of hand-washing and equipment sterilization facilities, within the patient care zone and at nursing stations in the layout of the rooms.
c. By providing both Positive Isolation Rooms and Negative Isolation Rooms.
Disease outbreaks can turn into major epidemics if well-designed isolation facilities are unavailable until permanent curative measures are discovered. It is extremely vital for healthcare institutions to be well prepared.
Kshititi Nagarkar,
Principal Architect, Shree Designs – Healthcare Architects & Planning Consultants
4. Keep it Airy
It is essential to work with the facility’s HVAC (Heating, Ventilation, and Air Conditioning) provider to implement filtration systems that match the layout, clinical goals and infection control policies of the healthcare organization. High-Efficiency Particulate Air (HEPA) filters, fixed into the HVAC systems, are often used in special-care areas. Air from airborne infection isolation rooms should be exhausted directly to the outside or be filtered through a HEPA filter, to prevent contamination of the other areas in the hospital.
5. Keep the Distance!
With the rise of communicable diseases, social distancing, which was always an aspect of community healthcare, is now needed as a part and parcel of patient-centred care, as it plays a big role in infection prevention and control in hospitals.
Generally, a well-designed healthcare institution would have incorporated the basic principles of social distancing in areas occupied or frequented by patients, like the wards, rooms and intensive care departments. However, due thought must be given to implementing these principles additionally in other areas like doctor consultation rooms, counselling spaces, waiting for spaces and so on. A few ideas to maintain adequate distance include:
- Closed counters with physical barriers like glass or plastic windows in receptions and billing desks can be used to avoid close contact with potentially infected patients.
- Seating arrangements must be a combination of individual seats, separated by tables or planters and isolated pods seating 2 to 3 persons in each pod. This will prevent the people from gathering together.
- The physical distance between the patients can be increased by planning seating arrangements with a minimum of 35 sq. ft. (3.25 sq. m.) per person and a maximum of 50 sq. ft. (4.65 sq. m.) per person.
- Horizontal circulation spaces can be increased to make up 22.5% – 30% of the area of the hospital.
Simply put, healthcare institutions need to be spacious, and their daily operations need to be streamlined to facilitate social distancing. Where space is at a premium, it is very challenging to put together administrative systems and align the design parameters with this paradigm shift, which will be a norm in the coming time.
At Shree Designs, we were entrusted with the project of redesigning our client’s existing Catheterization lab (Cathlab) while adhering to enhanced infection control and safety norms along with upgrading the medical equipment. Check out the complete project linked here: https://www.shreedesigns.in/project/cathlab-in-ussh-mumbai/

Stringent infection prevention and control measures in hospitals are rapidly becoming the norm in a post-pandemic world, as the healthcare industry evolves with time. An expert in healthcare facility planning will certainly make it easy for you to comply with accreditation standards and reduce the transmission of infections with the right support and design!
Related Posts
Colour Me Healthy!
The use of colour in hospitals and healthcare settings is an important aspect of patient recovery.…
The changing face of healthcare design
After completing a decade in designing healthcare projects, Kshititi Nagarkar, principal architect,…
Cost-effective and patient-centric hospital design
Biltrax Media in its Feb 2022 issue, published an interview with our principal architect Kshititi…
Patient-Centred Care and Community Healthcare
Patient-centred care focuses on individual patients’ healthcare needs and desired health related…
Social Distancing
Social distancing, a concept that has been around for ages, is one of the most vital measures…
Retrofitting For Healthcare Facilities
The word “retrofit” as we are aware suggests fitting in or on to an existing structure OR to…






