Why hospitals must be built not just for the patients who sleep, but for the teams who stay awake to protect them
Hospitals never truly rest. When the last outpatient leaves, when the corridors fall silent, and when patient wards dim into a soft hum of machines and breathing, another world inside the hospital begins its shift. Night-shift nurses, resident doctors, technicians, emergency teams, and support staff take over, carrying the responsibility of keeping every ward, every ICU, every emergency bay functional while the rest of the city sleeps.
Yet, the built environment around them is almost always designed for the day.
Night-shift healthcare design is rarely spoken about, but it determines staff alertness, patient safety, and the emotional well-being of the people who serve through the toughest hours. A hospital that works well at 2pm. must also work well at 2am, and both realities need different forms of support.
Ar. Kshititi Nagarkar, Principal Architect, Shree Designs
Designing healthcare spaces for night-shift workers is not simply about brighter lights or quieter hallways. It is about understanding the human body’s natural rhythms, the psychological weight of nighttime care, and the operational vulnerabilities that appear only after sundown.
It requires an architect who thinks like a clinician: precise, empathetic, and prepared for every variable.
The Hidden Physiology of the Night Shift
The human body is biologically programmed to wind down after sunset. Melatonin rises, heart rate slows, and cognitive sharpness naturally declines. But inside a hospital, the most critical decisions, emergency interventions, and error-prone procedures often occur between midnight and dawn, exactly when the body is least prepared. This mismatch between biology and responsibility is where architecture must intervene.
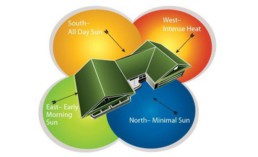
Lighting becomes the first line of defence. Staff zones need cooler, alerting illumination to counter circadian dips, while patient areas must remain warm and calming to protect rest. The right lighting strategy, tuneable LEDs, layered illumination, and glare-free surfaces allow hospitals to run in “dual mode,” supporting two different physiological needs at once.
But lighting is just the beginning.
Designing Workflows That Carry the Weight of the Night
Night shifts have fewer people on duty but more responsibility per person. Corridors are quieter, but emergencies feel louder. A single nurse may monitor multiple beds; a lone technician may run diagnostics; a duty doctor may be covering entire floors. This shift in dynamics demands healthcare interiors that reduce friction and amplify visibility.
Centralised nursing stations, for instance, allow a smaller team to maintain control over larger zones without constant walking. Glazed partitions, glare-controlled cove lighting, and open sightlines ensure staff can observe patients without disturbing them. Materials that absorb noise rather than amplify it prevent nighttime sounds from becoming jarring. The psychology of the built environment pulls significant weight here.
When space is calm, intuitive, and sensorially balanced, staff fatigue reduces — and patient safety improves.
Spaces That Support the Humans Behind the Night Shift
Night-shift workers don’t just need efficiency. They need refuge.
The emotional and cognitive load accumulated between midnight and 6 a.m. is unique. The silence can feel heavy. The lack of natural cues can disorient. Long stretches without interaction can deepen fatigue. Good hospital design creates small pockets of restoration without compromising readiness.
- A quiet room near critical care.
- A micro-rest zone with warmer lighting and ergonomic seating.
- A pantry corner that feels like a momentary escape rather than a sterile utility room.
- A few touches of biophilia or textured surfaces that soften the clinical environment.
These details are not indulgences; they are psychological safety nets. Even a few minutes of recovery in a thoughtfully designed staff area can restore alertness and reduce the risk of clinical error.
Safety After Sundown: The Other Half of Night-Shift Design
Nighttime introduces a different set of operational vulnerabilities: unauthorised entry, poorly lit movement routes, blind corners, sluggish emergency response, and limited backup personnel. – Design must anticipate these.
Secure access points, visible circulation spines, illuminated pathways from parking to staff entrances, and clear emergency signage ensure that the hospital remains as safe at 3 a.m. as it is during peak OPD hours. Even fire safety gains new significance at night — when fewer people are present and immediate help is not always at hand.
With the right healthcare architectural planning, the night shift becomes safer, calmer, and significantly more efficient.
Sustaining Long-Term Wellbeing for Night-Shift Teams
Chronic night-shift work affects stress levels, sleep cycles, cardiovascular health, and mental resilience. Healthcare architecture and design cannot change biology, but it can soften the strain. Circadian-aware light, restorative staff zones, acoustically controlled rest pockets, intuitive night workflows, and wellness-aligned materials all become tools to protect the very people protecting patients.
“Healthcare spaces must care for caregivers too,” says Kshititi. “A night-shift nurse navigating a dim corridor, a resident reviewing charts at 4 a.m., or a technician running late-night tests deserves a space that supports their body, their mind, and their duty.”
The Shree Designs Lens
At Shree Designs, we have always believed that healthcare architecture must serve every hour, every shift, every human who enters the building.
If you’re rethinking your facility or planning a new one, the Shree Designs team can help you build spaces that support not only patient care but the caretakers themselves.
Related Posts
Designing Healthcare Facilities
The Science of Hospital Windows
Windows in hospitals do far more than bring in light; they influence recovery rates, infection…
Infographic,Designing Healthcare Facilities
How Design Impacts Patient Care
Ever wondered what goes into designing a hospital or clinic that truly works - for doctors, staff,…
Designing Healthcare Facilities
Textures in Healthcare Spaces
When designing hospitals or clinics, texture is often seen as a “finishing touch.” At Shree…
Infographic,Designing Healthcare Facilities
The Lifecycle of a Healthcare Facility Design
Ever wondered what goes into designing a hospital or clinic that actually works - clinically,…
Designing Healthcare Facilities
Designing NABH-Compliant Hospital Interiors
A well-designed hospital isn’t just about aesthetics. From fire safety and infection control to…
Designing Healthcare Facilities,Infographic
Blueprint for Healthcare Design
From room dimensions to lighting levels, every detail matters in healthcare design. At Shree…
Designing Healthcare Facilities
Building Better Day Surgery Centres
Efficient care, happier patients, and smarter workflows - this is what defines a successful…
Project Management,Designing Healthcare Facilities,Infographic
Designing Healthcare Spaces That Truly Heal
From concept to completion, every medical space we design prioritizes patient flow, staff…
Designing Healthcare Facilities
The Business of Wellness
In the $1.8 trillion wellness industry, first impressions matter. Patients don’t just choose a…
Designing Healthcare Facilities
Efficient Hospital and Clinic Design
India’s emerging cities are growing rapidly, creating an urgent demand for accessible and efficient…
Designing Healthcare Facilities
Creating Calming and Confidential Spaces for Fertility Clinics
As the demand for fertility treatments grows, the architecture of these clinics plays a vital role…
Designing Healthcare Facilities
Designing the Perfect Hospital Pharmacy
Hospital pharmacies are the backbone of seamless patient care. From efficient workflows to secure…
Designing Healthcare Facilities
Preventive Care Facility Design Strategies
With preventive care emerging as the future of healthcare, this post outlines key architectural…
Designing Healthcare Facilities
Thermal Comfort Decoded
Thermal comfort plays a critical role in patient recovery, staff productivity, and overall…
Designing Healthcare Facilities
Building for Tomorrow: The Imperative of Adaptable Healthcare Design
Healthcare facilities need to be as dynamic as the industry itself. Traditional, rigid designs can…
Designing Healthcare Facilities
Designing Single Speciality Healthcare Centres
As single-speciality centres grow, their design needs become more specific, calling for tailored…
Designing Healthcare Facilities
Innovative Design Solutions for Senior Care Facilities
Designing senior-friendly spaces in healthcare facilities is crucial for catering to the evolving…
Designing Healthcare Facilities
Designing a Dental Clinic for Success
Providing quality dental care is not just about the technical elements of the treatment. It's also…
Designing Healthcare Facilities
3 Essential Design Features for Intensive Care Units
ICUs are not just limited to single units housing all critical patients. If the facility has…
Designing Healthcare Facilities
3 Lessons Learned While Building a Cardiac Cath Lab
Cardiac care design is moving at the sound of a new beat! The number of Cath labs in India has…
Designing Healthcare Facilities
5 Essential Elements of Healthcare Design
Design makes a significant impact on the delivery of care for both healthcare providers and…
Designing Healthcare Facilities
5 Best Ways to Create Healing Spaces for Kids
Designing spaces in healthcare facilities tailor-made for children is a lesson in balance! A…
Designing Healthcare Facilities
Top 5 Trends in Healthcare Design
Design can make all the difference when it comes to improving patient care. From a patient’s point…
Designing Healthcare Facilities
The Architectural Design of Hospital Facilities
Shree Designs designed and executed many efficient and safe healthcare setups in the middle of the…
Designing Healthcare Facilities
Dauntless Designers
Healthcare Radius in its 7th Anniversary Special issue in October 2019, featured a "power list of…
Designing Healthcare Facilities
The changing face of healthcare design
After completing a decade in designing healthcare projects, Kshititi Nagarkar, principal architect,…
Designing Healthcare Facilities
Thumb Rules for Planning and Designing of Hospitals
Traditional rules of thumb in healthcare planning have changed. Once-accepted rules can now be the…